Sepsis is one of the leading causes of death worldwide, causing one in every five deaths—about 11 million people each year. Yet, for being such a significant problem, it receives surprisingly little attention from the public.
Most people do not know how to recognize or respond to a sepsis infection, and many healthcare professionals are continuing flawed practices that perpetuate the problem, especially related to diagnosing and treating the condition. To help resolve this, let’s go over the basics of sepsis: its symptoms and effects, its roots, and what can be done to address it.
About Sepsis
Sepsis is an extreme, life-threatening response of the body to an infection. If left untreated, it can quickly cause tissue damage, organ failure, and death. Nearly any kind of infection can lead to sepsis. It can be identified by the following symptoms:
- High heart rate or weak pulse
- Fever, shivering, or feeling very cold
- Confusion or disorientation
- Shortness of breath
- Extreme pain or discomfort
- Clammy or sweaty skin
Sepsis has an extremely high mortality rate, and one in three people who die in a hospital have sepsis during their hospitalization. In addition to the risk of developing sepsis during hospitalization for an infection or surgery, those who are immunocompromised, such as cancer patients, have a higher risk of experiencing sepsis.
Today’s Sepsis Crisis
The main issue today is the proper diagnosis and treatment of the condition. “It can take a very long time to get a definitive diagnosis,” says Dorottya Nagy-Szakal, MD, PhD, Chief Medical Officer at Biotia. “About a third of patients don’t ever get diagnosed, and physicians will prescribe antibiotics without a diagnosis. With infectious disease, it’s very critical to get a definite answer within a certain time, because the pathogen needs the right antimicrobial therapy to be treated.”
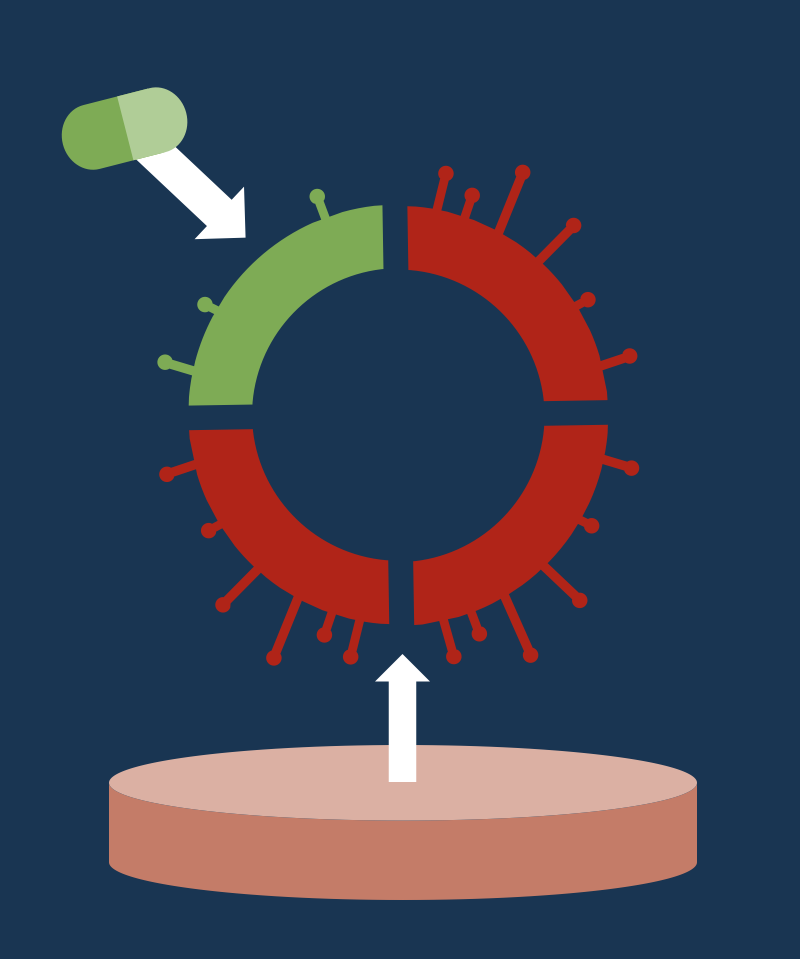
Sepsis can be the result of various pathogens, so it is important to identify the specific strain in order to prescribe the most effective antibiotic treatment. Physicians will often skip the diagnosis and merely prescribe an antibiotic, but this practice perpetuates what is known as “antibiotic resistance,” in which bacteria become nonresponsive to antibiotic treatment. Some scientists predict that by 2050, 10 million people will die from infections we don’t have treatment for due to this drug resistance.
What Can Be Done
A key to addressing these core issues of diagnosis and treatment is improving the diagnostic technology for faster, more accurate results. Biotia has developed and validated a next-generation sequencing-based assay with proprietary software and database to identify the specific bacteria species causing infections leading to sepsis. Biotia is working to bring this technology to the forefront of the healthcare system in order to more accurately diagnose and treat the condition.
In addition, Dr. Nagy-Szakal pushes the concept of “antibiotic stewardship”: that healthcare practitioners need to be more mindful and cautious when prescribing antibiotic treatment, ensuring that diagnosis is performed as quickly and accurately as possible before selecting the best treatment option.
Further, in response to this sepsis crisis, the World Health Organization (WHO) urges the global community to
- improve study designs and data collection on sepsis;
- increase global advocacy, funding, and the research capacity for evidence on the true burden of sepsis;
- improve surveillance systems and leverage existing programs and disease networks;
- develop rapid, affordable, and appropriate diagnostic tools to improve sepsis identification, surveillance, prevention, and treatment; and
- better educate health workers and communities on the risk of infections evolving to sepsis and the importance of seeking care promptly.
Whether you are a healthcare practitioner or not, you can use your increased awareness of the sepsis crisis to make a difference. If you are a patient, be proactive in requesting a sepsis diagnosis as soon as you are experiencing symptoms of a worsening infection. If you are a physician, use your “antibiotic stewardship” mindfully to make wise decisions based on accurate results. And be sure to implement the latest diagnostic technology into your practice. With everyone taking small actions to make a change, we can make a significant difference in improving health and saving lives across the globe.
Subscribe to newsletter
Subscribe to receive the latest blog posts to your inbox every week.